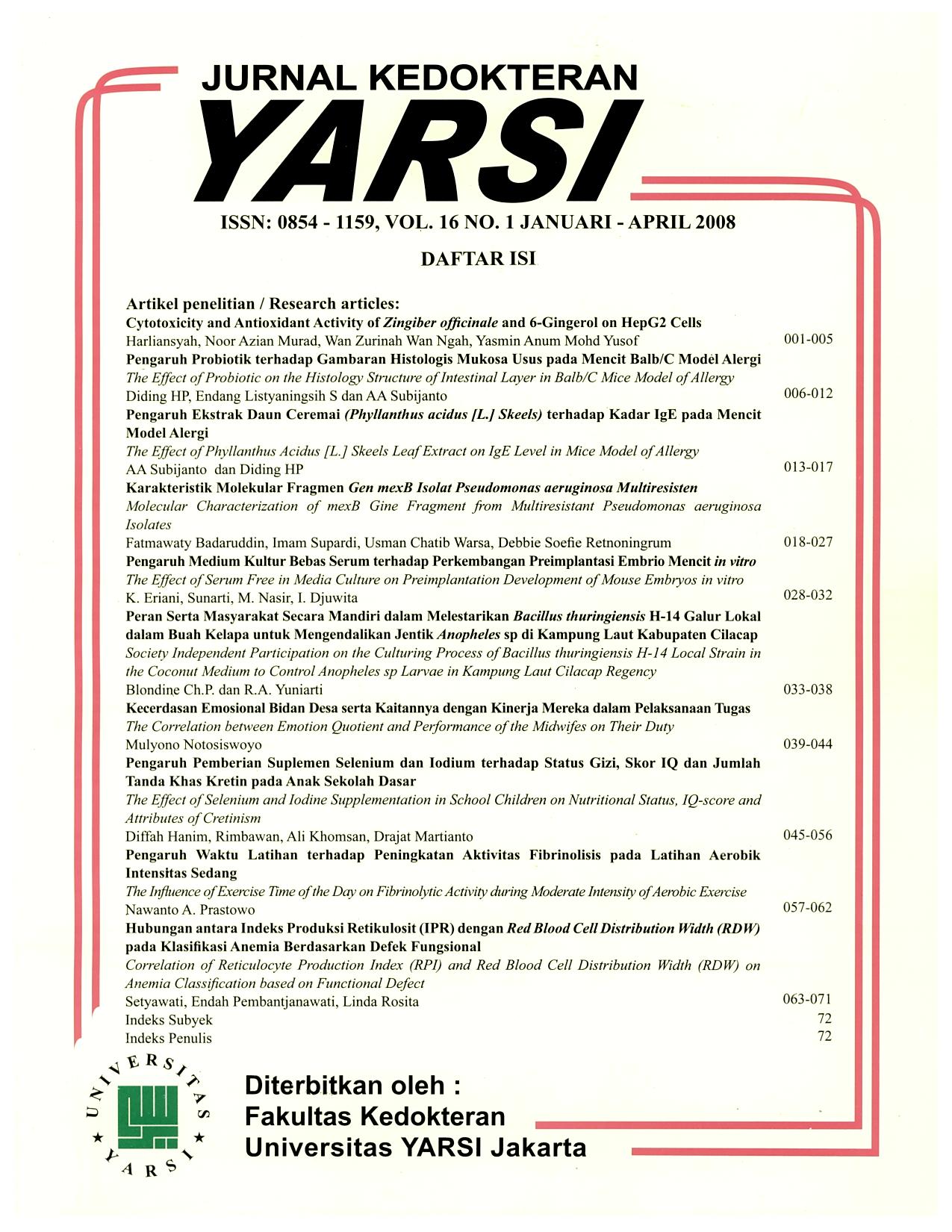
Karakterisasi Molekular Fragmen Gen mexB Isolat Pseudomonas aeruginosa Multiresisten
Keywords:
antibiotic resistant, efflux pump, sensitivity test, substrate recognition siteAbstract
Antibiotics have been widely used in the treatment of infectious diseases. However, their effectiveness has been questioned due to the tendency of some bacterial resistance to antibiotics. Pseudomonas aeruginosa among others has been known to be resistant to several antibiotics due to its MexABOprM efflux pump. Perhaps, the nucleotide sequence of its mexB gene fragment has changed followed by changes in amino acid sequence leading to alteration of the substrate recognition site. This alteration causes disability of antibiotics to recognize it and they are pumped out from the bacterial cell causing decrease in its inhibition concentration. An observasional study was performed using four P. aeruginosa isolates (A,B,C and D) taken from four laboratories in Bandung, and the sensitivity test for several antibiotics (tetracyclin, ampicyllin, amoxicyllin-clavulanat, kanamycin, ciprofloxazin, trimetoprim-sulphametoxazol, chloramphenicol dan eritromycin), was performed using Kirby-Bauer method. The Minimum Inhibitory Concentrations (MICs) for 4 isolates were 20.57-39.07 mg/ml for erithromycin, 29.35-48.57 mg/ml for kanamycin, 30.35-68.75 mg/ml for tetracyclin, 45.57-97.50 mg/ml for ampicyllin, 23.69-97.50 mg/ml for chloramphenicol, 25.82-59.56 mg/ml for amoxcyllinclavulanat,21.88-79.00 mg/ml for trimetoprim sulphametoxazol, and 20.58-56.97 mg/ml for ciprofloxazin. The increasing of MIC to each antibiotic was shown for 4 isolates of P. aeruginosa multiresistant to several antibiotics being studied. PCR technique was used to detect mexB gene fragment asumed as the substrate recognition site. The percentage of homology between the nucleotide sequence of mexB multiresistant P. aeruginosa and mexB P. aeruginosa producing siderophore pioverdin (Acc. No. L11616, NCBI) showed 96%, 100%, 97%, and 96% homology for P. aeruginosa A,B,C and D respectively. Employing DNAstar program, fragment variant of mexB gene of 4 multiresistant isolates A, B, C and D was detected. This variation lead to amino acid substitution of Gly-417->Ser, Glu-417->Gln, Thr-424->Pro, Tyr-328->Phe, Asp-328->His for P. aeruginosa A,B,C and D respectively, along with the change of their secondary structure, that changed the functional protein of MexB.References
Alonso A, Campanario E, Martines JL 1999. Emergence of multidrug-resistant mutants is increased under antibiotic selective pressure in Pseudomonas aeruginosa. Microbiology; 145(Pt 10):2857-62.
Barriere SL, Jacobs RA 1995. Clinical use of antimicrobial In; Basic and Clinical Pharmacology. 6 th. A Lange Medical Book,1995; 752-768.
Burns JL, Wadsworth CD, Barry JJ and Goodall CP. Nucleotide sequence analysis of a gene from Burkhoderia (Pseudomonas) cepacia encoding an outer membrane lipoprotein involved in multiple antibiotic resistance. Antimicrob. Agents Chemother. 40 : 307-313.
Carmeli Y, Nicolas T, George ME, and Mathew HS 1999. Emergence of antibiotic-resistant Pseudomonas aeruginosa comparison of risk associated with different antipseudomonas agents. Antimicrob Agents Chemother; 43:1379-82.
Evans K and Poole K 1999. The MexA-MexB-OprM multidrug efflux System Pseudomonas aeruginosa is growth phase regulated. FEMS microbiol Lett. 173 : 35-39.
Eda S, Yoncyama H, Nakae T 2003. Function of the MexB EffluxTransporter Divided into Two Halves. Biochemistry; 42(23):7238-44.
Elena B, Tikhonova, Qutju W and Helen I 2002. Chimeric Analysis of the Multicomponent Multidrug Efflux Transporter from Gram-Negative Bacteria. Journal of Bacteriology; 184(23)6499507.
Gotoh N 2001. Antibiotic resistance caused by membrane impermeability and multidrug efflux systems. Nippon Rinsho; 59(4):712-18.
George AM 1996. Multidrug Resistance in enteric and other Gramnegative bacteria. FEMS Microbiol Lett;139(1):1-10.
Guan L, Michael E, Hiroshi Y and Taiji N 1999. Membran topology of the xenobiotic-exporting subunit MexB of the MexA,B- OprM. Extrusion pump in Pseudomonas aeruginosa. J Biol Chem; 274: 110517-22.
Hancock RE 1998. The bacterial outer membrane as a drug barrier. Trends Microbiol. 5(1):37-42.
Li XZ, Zhang L, Poole K 2000. Interplay between the MexABOprM multidrug eflux system and the outer membrane barrier in the multiple antibiotic resistance of Pseudomonas aeruginosa. J. Antimicrob. Chemother.45; 433-436.
Levy SB 1992. Active efflux mechanism for antimicrobial resistance. Departemen of Mol. Biol. Microbiology and Medicine. Tufts school of Medicine, New England Medical Center Boston, 36: 695-703.
Masuda N, Gotoh N, Ishii C, Sakagawa E, Ohya S, Nishino T 1999. Interplay between chromosomal beta-lactamase and the MexAB-OprM efflux system intrinsic resistance to betalactams in Pseudomonas aeruginosa. Antimicrob. Agents Chemother; 43 (2):400-2.
Masuda N, Sakagawa E, Ohya S, Gotoh N, Tsujimoto H, Nishino T 2000. Substrate specificities of MexAB-OprM, MexCD-OprJ, and MexXY-OprM efflux pumps in Pseudomonas aeruginosa. Antimicrob Agents Chemother; 44(12):3322-7.
Morshed SR, Lei Y, Yoncyama H, Nakae T 1995. Ekspresion of genes yang associated with antibiotic extrusion in Pseudomonas aeruginosa. Biochem Bophys Res Commun; 210(2):356-62.
Ma D, Cook DN, Hearst JE and Nikaido H 1994. Efflux pumps and drug resistance in Gram-negative bacteria. Trends Microbiol; 2(12):489-93.
Mao W, Warren MS, Lee A, Mistry A, Lomovskaya O 2001. MexXY-OprM efflux pump is required for antagonism of aminoglycosides by divalent cations in Pseudomonas aeruginosa. Antimicrob Agents Chemother; 45(7):2001-7.
Murata T, Kuwakaki M, Shin T, Gotoh N, Nishino T 2000. The substrate specificity of tripartite efflux systems of Pseudomonas aeruginosa is determined by the RND components. Antimicrob. Biochem Biophys Res Commun. 299(2);2 74-51.
Nikaido H 1998. Multiple antibiotic resistance and efflux. Curr opin Microbiol. Okt,1(5): 516-23
Nikaido H 2001. Preventing drug acces to target : cell surface permeability barriers and active efflux in bacteria. Semin Cell Dev Biol; 12(3): 215-23.
Nakajima A, Sugimoto Y, Yoncyama H and Nakae T 2000. Lokalization of the outer Membrane subunit OprM of resistance-nodulation- cell division family multicompenent efflux pump in Pseudomonas aeruginosa. J Biol Chem; 275(29):1-11
Nguyen VJC, Gutmann L 1994. Resistance to antibiotics caused by decrease of the permeability in Gram-negative bacteria. Presse Med.; 23(11):522-31.
Nakae T 1997. Antibiotic extrusion and multidrug resistance. Nippon Rinsho; 55(5):1173-8.
Panzig B, Schroder G, Pitten FA, Grundling M 1999. A large outbreak of multiresistant Pseudomonas aeruginosa strains in north-eastern Germany. J Antimicrob Chemother; 43:445-18.
Paulsen IT, Brown MH and Skurrey RA 1996. Proton-dependent multidrug efflux systems, Microbiological Reviews; 60(4):575608.
Persing DH, Smith TE, Tenover FC, and White TJ 1993. In vitro nuc-leic acid amplification techniques, diagnostic molecular microbiology: Mayo Foundation Rochester 1993; 51- 87.
Poole K, Krebs K, Nelly MC and Neshad 1993. Multiple antibiotic resistance in Pseudomonas aeruginosa : evidence for involvement of an efflux operon . J Bacteriol. 175(22). 7363-73.
Poole K, Gotoh N, Tsujimoto H, Zhao QX, Wada, A Yamasuki T, Neshat S, Yamagishi JL, Li XZ, and Nishino T 1996. Overexpression of the mjexC-mexD-OprJ efflux operon in nfxB-type multidrug-resistant strain of Pseudomonas aeruginosa. Mol. Microbiol. 21(4) : 713-724.
Poole K, Srikumar R 2001. Multidrug efflux in Pseudomnas aeruginosa componenets, mechanisms and clinical significance. Curr Top Med Chem 1(1):59-71.
Zhao Q, Zin-Zhi L, Ramakrishnan S and Keith P 1998. Constribution of outer membrane efflux protein OprM to antibiotic resistance Pseudomonas aeruginosa independent of MexAB. Antimicrob. Agents Chemother; 42:1682-88.
Poole K 2002. Outer membranes and efflux: the path to multidrug resistance in Gram-negative bacteria. Curr Pharm Biotechnol; 3(2):77-98.
Pechere JC, Michea-Hamzhepour M, Kochler T 1998. Antibiotic efflux, a mechanism of multiple resistance in Pseudomonas aeruginosa. Bull Acad Natl med; 182(3):599-612.
Piddock IJ 1995. Mekanisms of resistance to fluoroquinolone. Drugs. 49(Supp 2):29-35.
Russell AD and Chopra I 1990. Understanding Antibacterial Action and Resistance. New York: Ellis Horwood.
Rubinstein E 199. Antimicrobial resistance-Pharmacological solutions. Infection; 27 Suppl 2:S32-4.
Sande MA, Kapusnik-Uner JE, Mandell GL 2000. Antimicrobial Agents : General Consideration. In : Goodman & Gilman, A. et al. eds. Pharmacological basis of Therapeutic, 9th ed. Mc Graw-Hill; 1018-46.
Sastramihardja HS, Adinoto W, Sumadilaga RS, Widiaputri EA 1986. Tinjauan Farmakologi Antibiotika, Disinfektan dan Antiseptik. Naskah pada seminar dan lokakarya Penanggulangan Infeksi Nosokomial di RS Hasan Sadikin Bandung.
Saito K, Eda S, Maseda H, Nakae T 2001. Molecular mechanism of MexR mediated regulation of MexAB-OprM efflux pump_expression in Pseudomonas aeruginosa. FEMS Microbiol Lett;195(1):23-8.
Srikumar R, Li XZ, Poole K 1997. Inner membran efflux components are responsible for beta laktam specificity of multidrug efflux pumps in Pseudomonas aeruginosa. J Bacteriol; 179(24):7875-81.
Speciale A, Musumeci R, Blandino G, Caccamo F, Siracusa V, Renis M 2000. Molecular mechanisms of resistance in Pseudomonas aeruginosa to fluoroquinolones. Int J Antimicrob Agents; 4(2): 1516.
Lehninger AL 1982. Principles of biochemistry. USA: Worth Publishers; 107-131.
Zarifi IZ, L Catherine, K Thilo, P Jean-Claude and P Patrick 1999. In vivo Emergence of Multidrug-Reistant Mutant of Pseudomonas aeruginosa Overexpressing the active Efflux System MexA-MexBOprM. Antimicrob. Agents Chemotheraphy. 43 : 287-91.
 Fatmawaty Badaruddin
Fatmawaty Badaruddin
 Department of Pharmacology, Hasanuddin University, School of Medicine, Makassar
Department of Pharmacology, Hasanuddin University, School of Medicine, Makassar